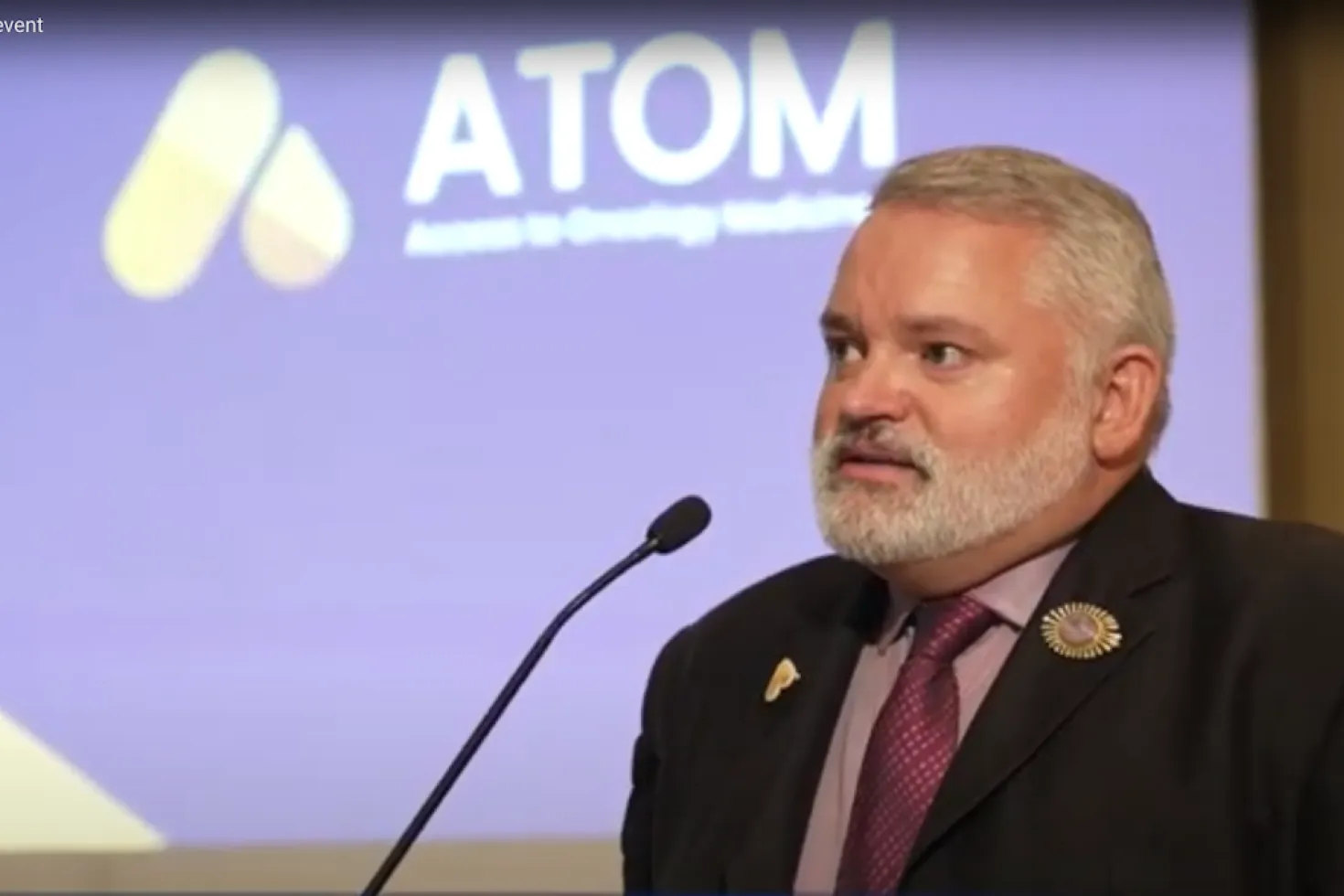
For every patient, everywhere: Dr Dan Milner
In this wide-ranging Q&A with Dr Dan Milner, the new Executive Director of the Access to Oncology Medicines (ATOM) Coalition dives deep into the issues affecting access to cancer medicines in low- and middle-income countries.
HIGHLIGHTS
-
There are many barriers that complicate access to essential medicines. To best addess these barriers, it is important to understand which barriers have solutions and who can enable those solutions.
-
Critical building blocks for a robust and resilient health system supporting equitable access to essential cancer medicines and diagnostics are knowledge and financing.
-
Clear opportunities to improve access include shifting the focus from profit to service provision, investing in education and training and developing a simpler, more harmonised registration process for medicines.
Dr Dan Milner is the former Chief Medical Officer of the American Society of Clinical Pathology (ASCP). He began working in Africa in 1997 as a medical student and has built an international reputation as an expert in cerebral malaria, and has spent 10 years at Harvard where he taught pathology, microbiology, and infectious disease.
Drawing from decades of experience improving cancer diagnostics and care, Dan discusses why a “quick win” is often an oxymoron in cancer care, how knowledge is critical (but also comes with great responsibility), the one incontrovertible fact that patients are at the centre of everything, and much more.
What are some of the issues that complicate access to essential cancer medicines and diagnostics, particularly in LLMICs?
There are many barriers – perhaps the more important question is: "Which barriers have which solutions and who can enable those solutions?"
Lack of time, money, or knowledge, living remotely, fear of a cancer diagnosis, and personal experiences with the healthcare system are some of the challenges that many people face in obtaining the appropriate medicines. By simply making medicines free or at a very low cost does not overcome all the barriers for every patient.
An important part of the solution is to enable primary care, community healthcare workers, friends and family, and advocates, to provide all potential cancer patients with a support network. This is as important, if not more important than financial access to care.
Then there is a lack of resources to screen patients, which could be addressed systematically by developing specimen transport networks and reagent and supply access. Overcoming other barriers inherent in the health system itself – such as limited knowledge about oncology and the referral services that are available, and/or a lack of support for patients to move through their cancer journey – require a different solution, including education and training.
In diagnosing cancers, there are challenges that relate to laboratory and radiology services. To treat cancer, we are up against barriers relating to the availability and affordability of the different treatment modalities, including medicines, surgery, and radiation oncology. Similarly, in providing supportive care, the availability and affordability of services such as social support, palliative pain management, survivorship support, and end-of-life care, also present challenges.
Through the ATOM Coalition, we are focusing on the medicines access component of this complex cancer continuum, while recognising that all parts must be addressed.
One cannot imagine a single organisation that could handle all these challenges. An integrated cancer care approach, with support from multiple organisations, could formulate a solid set of solutions.
Where has the global cancer community been weakest in addressing access and availability? What have been notable areas of progress?
There is a critical need to address GDP-based/tiered pricing of all reagents, supplies, equipment, etc., which are essential to support cancer diagnosis and treatment. Take, for example, the fact that most diagnostics are manufactured in high-income countries, whose markets are other high-income countries. Given that diagnostic companies’ margins are considerably lower than pharmaceutical companies, diagnostic companies generally do not have the fiscal bandwidth to reduce their prices with the current model. This means that prices of cancer diagnostic supplies are often outside the reach of lower income countries.
However, we can take the lessons learned from HIV, malaria, and COVID-19, where the manufacture of diagnostics is close to the location of use—for example, manufacturing in Africa for African countries. This helps to drastically reduce the costs of diagnostics, as well as eliminate import tariffs, taxes, customs charges, while reducing time to supply chain completion.
One possible mechanism to address this market imbalance in pricing is through regionalised purchasing. The PAHO Strategic Fund offers a good example of this, where pooled procurement of essential medicines, including for cancer treatment, is helping to strengthen access.
Some 20 years ago, I was sitting at a microscope in Malawi looking at surgical biopsies and seeing horrific cancers that were months old. At that time, there was only one surgeon available to read the report. Thankfully, this has changed. It’s an area where I have seen the biggest leap, that is the growing recognition of the roles of not only pathology and surgery, but of medical oncology, radiation oncology, and all supportive care modalities.
At the global and country levels, we have witnessed a dramatic increase in national cancer control plans thanks notably to the International Cancer Control Partnership. The creation of paediatric, cervical and breast cancer model programmes by the WHO has also been an outstanding leap forward, as have international resolutions focused on cancer – from the first on cancer prevention and control in 2005 to this year’s resolution on strengthening diagnostics capacity.
This is thanks in part to efforts of organisations like UICC and its member organisations in driving the global agenda. Through civil society, social impact groups, patient advocacy groups and people living with cancer themselves, the world is more keenly aware of cancer and that knowledge grows every day.
But with great knowledge comes great responsibility and the financial barriers and opportunities created by a strong will to identify and treat cancer await our permanent solutions.
What are the critical building blocks of a robust and resilient health system that supports equitable access to essential cancer medicines and diagnostics?
I see two critical elements of a strong health system: (1) Knowledge and (2) Financing. All stakeholders – from patients to healthcare providers from government to the public – must all be aware of cancer as a disease, understand that it can be prevented, screened for, and/or treated, and have realistic expectations about what can be achieved with what investment.
Universal health coverage (UHC) is an essential building block of an effective health system and is imperative in protecting an individual patient and their family from financial ruin due to a cancer diagnosis. Effective UHC integrates fiscal schemes that cover the unique needs of people living with cancer and adopts innovative models for support (e.g., community contributions schemes, cross-subsidisation, public and private insurance programmes, pro bono care qualifications mechanisms, voucher programmes, etc.).
In parallel, a national programme that prioritises and funds community-based activities (e.g., HPV vaccination, clinical breast exams, anti-smoking campaigns, educational programmes about paediatric cancer, etc.) must be part of any functioning health system.
What are the clear opportunities and quick wins that the global cancer community should be seizing when it comes to improving access to essential cancer medicines and diagnostics?
“Quick wins” is a bit of an oxymoron in global oncology for the most part because there are very few “simple” cancer problems.
The most straightforward cancer to diagnose and treat is chronic myeloid leukaemia (CML) and ATOM Coalition partner, the Max Foundation has created a brilliant approach to solve that disease globally – an example of an important and quick win. But as we move to more complicated cancers, these opportunities require a marathon and not a sprint.
Innovative ways to develop patient-centred cancer services are key. It is also essential to shift the focus from profit to service provision, while maintaining revenue streams that justify the investment. For example, an initial donation of reagents or funds to buy reagents at a negotiated and affordable price allows a lab to sell those tests at the local rate, receive the revenue, and still have sufficient funds to purchase new reagents; thus, the lab can sustain and grow the service without ongoing fund donation.
One diagnosis-specific “quick win” is investment in training, education, and support for cytological diagnosis of cancer, as it creates an opportunity to triage patients for referral services or to reassure them about benignity. Because it is low-cost and can be enhanced by telecytology (which allows the diagnosis to be accessed remotely), it could allow screening approaches to observable and accessible lesions with or without costly ultrasound.
Finally, transforming the registration process for medicines to a simpler, collaborative, and more harmonised system would save enormous amounts of time and energy and more rapidly make medicines available. Also, the needs of patients who require pain management must take precedence over misconceptions and fears of diversion surrounding pain relief medicines such as opioids. Sadly, today we see an enormous amount of unnecessary suffering in late-stage cancer.
How is the ATOM Coalition uniquely addressing the issue of access to medicines and diagnostics (availability, accessibility, affordability, and acceptability)?
The unique approach of the ATOM Coalition is to call for, organise, and manage a collaborative, cross-sector approach to access for medicines and diagnostics. Many partners and collaborators have already “solved” their piece of the puzzle. But taking all those well-fitting puzzle pieces to scale in countries that have lacked concerted efforts towards their cancer programmes is where the ATOM Coalition should excel. Other initiatives such as The Max Foundation’s program to advance access for CML therapy and the American Society for Clinical Pathology’s (ASCP) cancer histology diagnostics initiatives have done partially what the ATOM Coalition is proposing for specific diseases, for specific types of gaps, or for a focused cancer in one domain.
That is the strength of the ATOM Coalition: learning from our partners and potential collaborators and creating novel solutions as needed for unique challenges in each target country.
Partnering and collaboration often present challenges and points of tension. With nearly 40 partners, how do you see the ATOM Coalition offering a successful way of working together?
Collaboration is not always the answer to every problem. Sometimes a situation requires a strong leader that can see the forest for the trees and mobilises the necessary forces to achieve success. For example, performing a play, building a house, or running a medical clinic.
But cancer is not that type of problem. People with cancer interact with more members of the medical community than the average patient. Each part of the cancer journey is critical to a better outcome. That’s why each component needs a strong leader and dozens of others to make it happen. But to truly build an efficient cancer programme, all the pieces must be aligned. Organising a group of strong leaders, each with their own area of expertise, can create a collaborative effort that works.
The important role of the ATOM Coalition is to make sure all viewpoints from each part of the cancer journey are represented, utilise expertise when it is needed for a given implementation plan, and foster accountability and transparency around what success looks like — focused on the patient’s outcomes.
The first-ever voluntary licence for a cancer medicine was announced in October last year, setting a promising precedent. What can be done to support more companies to consider VLs in the future and what will be the impact for LLMICs?
Voluntary licenses can create a win-win-win situation: for the originator, generic manufacturer, and the patients. For the originator, it offers a royalty revenue stream that can either be added to their bottom line or donated to support the ongoing infrastructure for procuring and utilising VLs. At the same time, VLs help remove costs associated with production, distribution, registration, etc. that come with directly manufacturing a medicine. For the generic manufacturer, the VL is utilised to produce a medicine at a much-reduced cost, allowing it to be affordable in target countries.
The very important point of this scenario is that, early on, the revenue stream may be small but as the programme grows and there are more VLs in more countries where more patients are being diagnosed and treated, this generates multifaceted ROI, including sustained positive publicity, high quality social capital, global brand access and awareness, economic development, transitioning of economies, and positive revenue flows to companies.
Investment in healthcare systems shown repeatedly, to massively improve and grow local economies in the towns around these health interventions. Partners in Health is a prime example. By providing affordable medicines through access mechanisms like VLs, companies are investing in the economy of these countries and providing a positive return on investment.
As the new Executive Director of the ATOM Coalition, what are your priorities?
A strategic plan for the ATOM Coalition for the next five years is essential. It must mobilise the strengths of our existing partners, easily identify the gaps we need to fill with new partners and resources and offer the most immediate impact for people with cancer.
Direct engagement with target countries to assess their needs, gaps, and immediate possible successes is also crucial. Another priority is exploring all the current models of access to identify opportunities for synergy and expansion through the ATOM Coalition. Finally, we will ensure an open dialogue with all current and future partners to identify all opportunities for success, eliminate redundancies and inefficiencies, and respond to emergent challenges.
In the longer term, what conversations should the global community be having about access?
If there is a medicine that will treat a patient’s condition, that person should have access to that medicine no matter who they are, where they were born, or how much money they have. Access to healthcare is a human right, not a privilege nor a luxury.
We must all recognise that a person who has cancer is not at fault. No one chooses to have cancer. It is a fallacy and a confirmed failure if we chose to approach, for example, lung cancer in a smoker differently than how we approach leukaemia in a child.
We must also accept the incontrovertible fact that patients are at the centre of everything we do in healthcare and especially in cancer care.
Nothing is of any value at all if the patient does not have the best possible outcome for their disease. That outcome includes inherently the best possible mental, physical, fiscal, and social situation.
Last update
Tuesday 11 April 2023
