Screening for change in lung cancer diagnosis: turning the tide with technology and trust
Ahead of World Lung Cancer Day on 1 August, UICC is highlighting the potential of detecting lung cancer earlier through low-dose CT screening and technological innovation – themes reflected in BBC StoryWorks films produced for the Rewriting Cancer series supported by UICC.
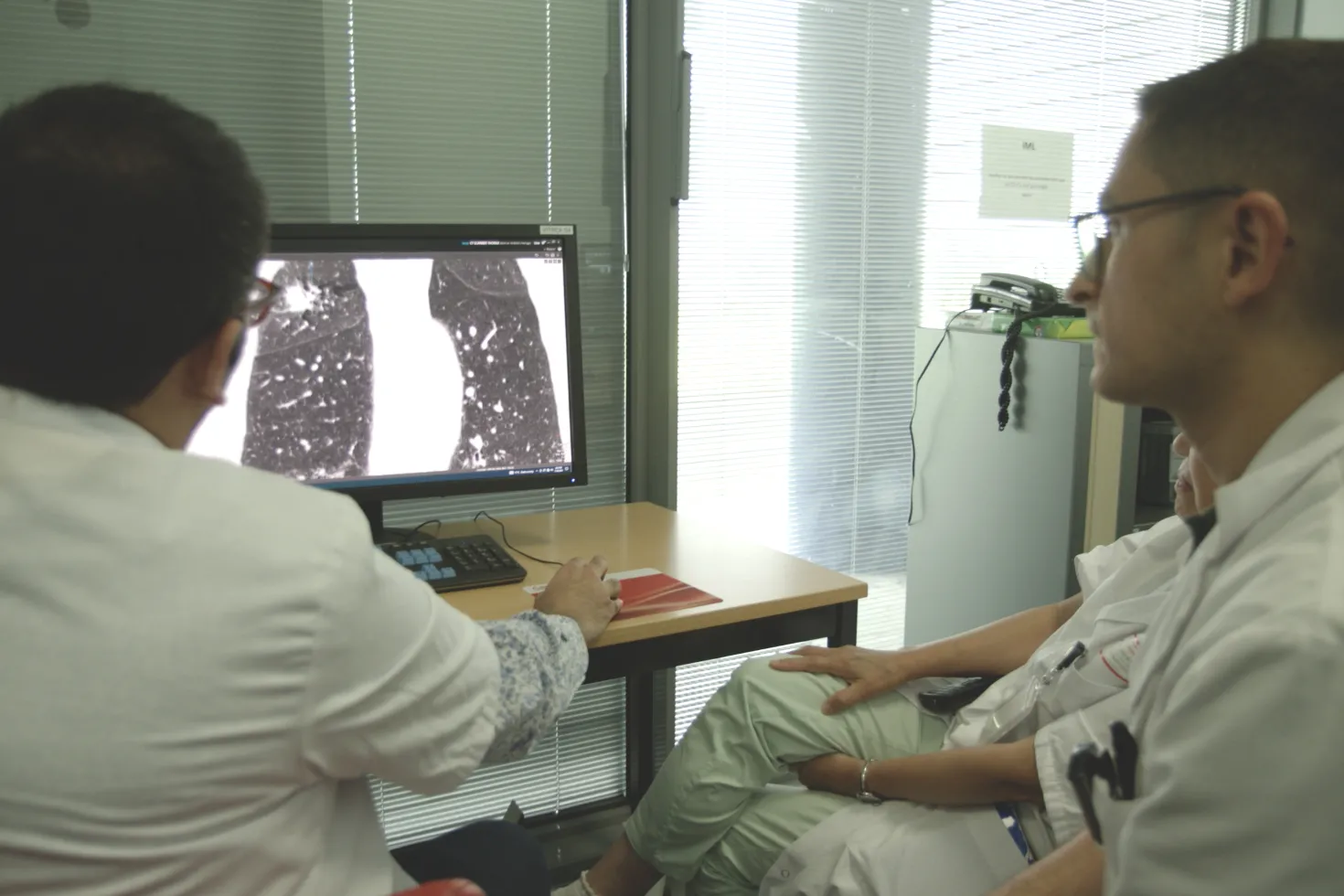
From the branded film "Detecting cancer earlier with AI – How better image quality can help detect early stage lung cancer", produced for Canon Medical Systems by BBC StoryWorks as part of the Rewriting Cancer series presented by UICC.
HIGHLIGHTS
- Because lung cancer is generally asymptomatic in the early stages, it is often detected late, and leads in the numbers of cancer cases and deaths, driven by tobacco consumption, air pollution, and other environmental causes.
- Widespread implementation of low-dose CT screening remains limited despite proven benefits.
- Mobile units, AI tools and national screening programmes are helping expand access.
Because lung cancer is typically asymptomatic in its early stages, detecting the disease early is critical to reducing deaths related to what remains the most commonly diagnosed and deadliest cancer worldwide (Globocan 2022).
At least a decade of evidence shows the benefits of low-dose CT scans as one of the most effective tools for detecting lung cancer early, when treatment is more likely to succeed.
Yet effective screening remains limited in many countries for reasons including cost, resource allocation, stigma surrounding lung cancer, and political will, with lingering doubts about the efficacy of low-dose CT scans in reducing lung cancer mortality.
Ahead of World Lung Cancer Day on 1 August, UICC spoke to leading voices in radiology and health innovation about how to shift the paradigm and implement effective, targeted population-wide screening programs that will save lives.
Australia launched its first national lung cancer screening programme on 1 July 2025, targeting long-term smokers aged 50 to 70. In the UK, the NHS Lung Health Check programme, which UICC reported on last May, offers lung health assessments and low-dose CT scans, via mobile scanners in community settings to people aged 55–74 who currently smoke or have done so in the past. These checks have already identified thousands of early-stage cancers and are being expanded nationally by 2030.
Another initiative aiming to address access and reach is a mobile lung screening programme highlighted in the short branded film ‘Detecting cancer earlier with AI’, produced for Canon Medical Systems by BBC StoryWorks as part of the Rewriting Cancer series presented by UICC. It features a van equipped with a low-dose CT scanner that travels to underserved areas in France, offering lung cancer screening free of charge.
This mobile screening programme is connected to the global initiative, ‘Screen for Life. Breathe with Hope’, which offers free low-dose CT scans to adults aged 50–75 with a significant smoking history. It aims to eliminate access challenges such as travel and cost, while alleviating hospital imaging demand using Canon Medical’s mobile CT units equipped with low-dose imaging and AI-assisted workflows.
“Bringing screening closer to people’s homes helps reach those who might otherwise never be tested,” said Prof. Mikhael Ohana, a radiologist based in Strasbourg who features in the five-minute short. “It’s about reducing logistical and psychological barriers – getting people in earlier, when intervention is still possible.”
Prof. Marie-Pierre Revel, also featured in the film, is both a radiologist and a lung cancer survivor. After losing her cousin to the disease, she was herself diagnosed early through a CT scan and successfully treated. She now leads the CASCADE study in France, which targets high-risk women and investigates whether single readings by general radiologists, supported by AI, can match the accuracy of double expert reviews. The study also looks at psychological outcomes, adherence, and cost-effectiveness.
AI in screening: Balancing innovation with trust
While the growing use of AI in clinical decision-making can raise concerns around trust, transparency and depersonalisation, Prof. Ohana emphasises how artificial intelligence can support radiology practice in clinical settings, with limitations. “AI can assist radiologists by highlighting lesions that may be missed in standard reads and help mitigate fatigue,” he said. “But it should be viewed as a support tool rather than a replacement. Human expertise remains essential, particularly with complex cases.”
This perspective is echoed in another film from the Rewriting Cancer series, ‘The AI ‘speed reading’ scans – Helping radiologists identify lung cancer’, produced by BBC StoryWorks for Deep Health, a health technology firm specialising in AI-powered diagnostic tools that enhance radiologists’ capacity to detect lung cancer. According to Sham Sokka, Chief Operating and Technology Officer at DeepHealth, the UK’s expansion of its NHS Lung Health Check has demonstrated how cloud-based AI tools can facilitate population-wide screening by speeding up image review while maintaining accuracy.
“AI supports radiologists in managing the high volume of scans involved in large-scale programmes,” Sokka explained. “In the UK, for instance, a full rollout means reading millions of scans. AI reduces that burden and allows clinicians to work more efficiently.”
Sokka also highlighted the importance of ensuring public trust in both AI and screening itself. “There’s stigma around lung cancer because of its association with smoking,” he said. “This can delay care or deter people from participating in screening. The challenge is to reframe it – early detection isn’t about judgement, it’s about giving people a chance.”
Overcoming the barrier of stigma, strengthening health system capacity
Prof. Ohana echoed this concern, noting that stigma can subtly influence both public perception and political commitment. “Mentalities have been changing, but lung cancer as it relates to smoking is still seen by many as a self-inflicted disease,” he said. “That perception can undermine support for screening programmes and deter people from seeking early care – even when they are eligible and would benefit.”
Blaming individuals for developing lung cancer overlooks a much broader reality. Health is shaped not just by personal choices but also by social and environmental conditions. And commercial interests of the tobacco industry that drives manipulative marketing tactics.
Furthermore, while smoking remains a leading cause, it is far from the only one. Outdoor air pollution as well as indoor pollution from cooking fuels and poor ventilation, are increasingly linked to lung cancer – particularly in never-smokers. In fact, rates of lung cancer among people who have never smoked are rising, especially in women and younger adults.
These findings challenge outdated assumptions and reinforce the need for inclusive, stigma-free approaches to screening and care.
Yet stigma is not the only barrier to screening and early care. Even in high-income settings, workforce shortages continue to limit screening capacity. Both Sokka and Ohana point to AI-supported workflows and mobile units as potential ways to alleviate pressure on existing systems.
In addition to detection, the value of screening also depends on what follows. Prof. Ohana noted that earlier-stage diagnosis increases the likelihood of less invasive and more effective treatment options, such as surgery or targeted therapy. “When lung cancer is found early, treatment can often be localised and curative,” he said. “But if we wait until symptoms appear, we are frequently dealing with advanced disease, where options are limited.”
At the global level, UICC leads the Lung Cancer Collaboration (LCC) – a multi-stakeholder effort that is supporting integrated approaches to lung health. “Screening is not just a clinical intervention; it’s an investment in people’s health and futures,” said David LeDuc of AstraZeneca, an LCC partner. “It helps to reduce treatment costs, improves outcomes, and supports families and communities.”
Despite the advances, many gaps remain. “We’ve had the tools for over a decade, the challenge is to align systems and policies to use them effectively,” said Ohana. “But technology alone isn’t enough. We have to change hearts and systems. Every delay means missed opportunities to intervene earlier and save lives.”
Last update
Tuesday 29 July 2025
