Marking World Lung Cancer Day during the COVID-19 pandemic
Lung cancer kills more than 1.7 million people each year, yet with proper prevention and accessible treatment these numbers can be reduced.

World Lung Cancer Day on 1st August provides an opportunity to raise greater awareness about the risk factors and patients’ outcomes of this deadly and debilitating disease, and review the prevention measures and treatment options that help reduce the global burden. Furthermore, because the ongoing coronavirus pandemic is marked by severe respiratory symptoms, lung cancer is an aggravating factor for COVID-19 and it is important to understand how to address these additional risks for patients.
Incidence and risks factors
Lung cancer is the leading type of cancer in the world, with more than 2 million cases and 1.7 million deaths in 2018. In 2040, the number of cases is expected to reach 3.5 million with an annual death toll of 3 million deaths worldwide. Smoking is, of course, a primary cause of lung cancer and the risk of developing it increases depending on how many cigarettes and for how long a person smokes, and well as the length of exposure to second-hand smoke.
There are, however, multiple other factors that trigger lung cancer. For instance, outdoor air pollution accounts for an estimated 15% of lung cancer deaths and indoor air pollution is also a contributing factor. Indoor pollutants include stoves, fireplaces, heaters (especially using coal and other fossil fuels) and chemical compounds such as asbestos and radon (radioactive gas).
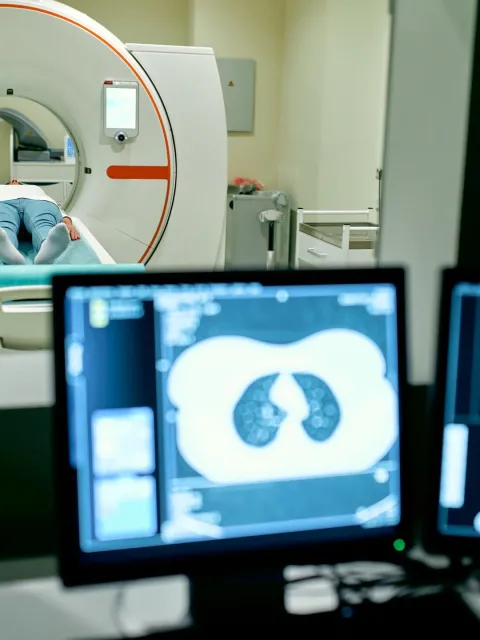
Current treatments for lung cancer
The two main types of lung cancer are small-cell lung cancer and non-small cell lung cancer (the most common). As with other types of cancer, different stages of lung cancer (from early diagnosis to advanced forms of the disease) require different treatments.
Surgery is performed to removed cancer tissues, while chemotherapy uses chemical compounds designed to limit the growth of cancer or eliminate it. Radiation therapy is used to kill cancer cells with high-energy rays. Another treatment consists of targeted therapy with customised drugs directed at specific biomarkers. These types of therapy can be chemotherapy or immunotherapy, the latter using antibodies that can target the tumour or support the immune system to kill the cancer cells.
Despite the plethora of treatment, however, and depending on the stage at which the lung cancer is diagnosed, the overall five-year survival rate of lung cancer ranges from 6% when cancer has spread outside of the lung (metastasized) to 60% when it has not.
Preventing lung cancer
Refraining from smoking and avoiding places where smokers can smoke indoor can largely reduce the risks of developing lung cancer – and public policy is an important tool for reducing smoking prevalence and enhancing public health.
"Exposure to second-hand smoke is not a choice, especially for children. It is the responsibility of governments to enact legislation to ensure healthy environments and protect people of all ages from the harms of tobacco smoke."
- HRH Princess Dina Mired, President, UICC
Germany, for instance, ranks last on the tobacco control scale and has taken few or no measures since 2010 (advertising on billboards are still allowed for instance ); smoking prevalence for persons aged 15 and older stands at 32.4%. The UK, on the other hand, ranks first with respect to key measures taken (plain packaging, high excise tax, a ban on smoking in cars when minors are present, and the ratification of the FCTC illicit trade) and boasts a far lower smoking prevalence at 19.9%.
It is also important to reduce the presence and use of other carcinogens and chemical compounds that trigger lung cancer. Governments and employers have a responsibility to provide safe public and working spaces for their citizens and employees. Each person should endeavour to lead a healthy lifestyle with a varied diet, including adequate portions of fruits, vegetables and whole grains. Regular physical activity has also been shown to lower the risk of many cancers including lung cancer.
Lung cancer patients in the time of COVID-19
Since the outbreak of the COVID-19 pandemic in early 2020, cancer patients have faced rising challenges in accessing health services. Indeed, cancer care to assist patients, relatives and caregivers is under pressure. Surgeries have been delayed and diagnosis and early detection have been postponed, either because health systems are overwhelmed or because patients are concerned about the potential effect on their health or treatment in case of a coronavirus infection and are afraid to consult a doctor. There are clear unmet needs for information, either on the patients’ side or for healthcare specialists.
“NCDs make us much more vulnerable to the ravages of coronavirus. (…) The single most effective tobacco control policy is increased taxation. When tobacco is more expensive, people use it less and quit more often. So at a time when governments are scrambling to find appropriate revenue schemes, higher taxation of tobacco products can offset the costs of public health and health care systems in general."
- HRH Princess Dina Mired, President, UICC and José-Luis Castro, Executive Director of The Union in 'Covid-19 and Tobacco: Unmasking the Smoke Screen'.
Last update
Wednesday 05 August 2020