Breaking barriers and improving access to cancer services for women in Africa
Marking International Women’s Day on 8 March, Dr Zainab Shinkafi-Bagudu spoke about the significant barriers to cancer care that women in Africa face due to cultural stigma, financial constraints, and limited healthcare access, and effective actions to bridge the gap.

HIGHLIGHTS
- Cultural stigma and misinformation discourage early cancer diagnosis and treatment, particularly for cervical cancer.
- Financial constraints and gender norms often prevent women from seeking medical care.
- Community-based advocacy and HPV vaccination initiatives are helping increase awareness and prevention.
- Expanding insurance, mobile screening units, and government funding improve healthcare accessibility in a sustainable manner.
Women across Africa continue to face significant barriers in accessing essential cancer services, with deep-rooted cultural beliefs, economic constraints, and logistical challenges limiting early diagnosis and treatment.
Dr Zainab Shinkafi-Bagudu, President-elect of UICC and Founder of the Medicaid Cancer Foundation in Nigeria, outlined how to address these challenges and improve healthcare for women in Africa on the occasion of International Women's Day, celebrated on 8 March.
What are the main challenges women in Africa face in accessing essential cancer services?
Cultural stigma remains one of the greatest obstacles. Misinformation and superstition surrounding diseases such as cervical cancer lead to resistance against life-saving interventions such as screening and vaccination. There is a lot of fear and misunderstanding about cancer. Many believe that a diagnosis is a death sentence, and this discourages them from seeking early treatment.
Are there any other cultural norms or social expectations for women that affect their ability to seek care?
Even when women are aware of the risks, cultural norms and social expectations often prevent them from seeking care or undermine their ability to do so. Many women, for example, are primary caregivers and often prioritise their families’ health over their own. If a mother has to decide between spending on herself or feeding her children, she will always put her family first. Furthermore, in many households, men control financial resources and women often cannot seek care without their husband's approval.
What role do economic constraints play in limiting access to cancer treatment for women?
Economic considerations and the fact that women are often not financially independent further complicate access. In countries where healthcare is largely paid for out-of-pocket, the cost of diagnosis and treatment is a significant barrier. A lot of women cannot afford cancer treatment.
What logistical challenges do women face in accessing cancer centres and treatment?
Logistical challenges also play a role and add to the financial burden. In Nigeria, 80% of cancer patients travel at least three hours to the nearest cancer centre. If you factor in transport costs, accommodation, and lost wages, it becomes clear why so many women delay seeking care or do not go at all.
What initiatives have proven effective in overcoming cultural resistance and improving awareness?
Community engagement has proven to be a key strategy in overcoming cultural resistance. When we work with the gatekeepers – traditional rulers, religious leaders, and male heads of households – when we have programmes that are in the languages that the people understand and involve not just the women but also the community gatekeepers, those programmes work best. Even though these institutions are male-led, once we have their buy-in, the impact on women’s health is enormous.
How can targeted education and awareness campaigns help in dispelling myths and promoting early screening?
Raising awareness through targeted education is also effective, such as training local advocates, religious leaders, and youth ambassadors. These actions have helped to dispel myths and promote early screening initiatives. Mentoring the next generation is key. We need more health advocates who understand local challenges and can provide solutions tailored to their communities.
What steps are being taken to ease the financial barriers to cancer treatment?
Various initiatives are being introduced to mobilise government commitment and funding, expand insurance coverage, and reduce out-of-pocket costs. Expanding coverage and subsidising cancer treatments in particular can significantly ease the burden on women who cannot afford medical care.
How crucial is improving healthcare infrastructure and accessibility?
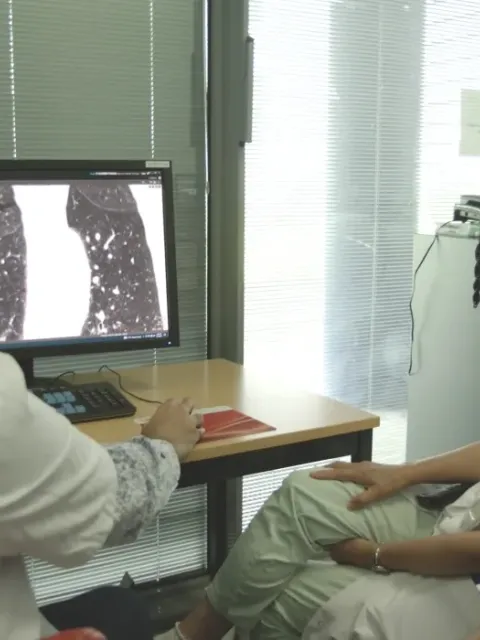
Improving healthcare infrastructure and accessibility is very crucial. More cancer screening centres are being established in rural and underserved areas to reduce the distance patients must travel. Mobile screening units and telemedicine services have also been introduced to bring diagnostic tools closer to communities. These as well as mobile health units and local screening programmes are helping to bridge the gap in access.
What is the Medicaid Cancer Foundation doing to address the situation and might be some lessons learned for organisations in other countries?
The Medicaid Cancer Foundation is tackling these challenges head-on by making cancer care more accessible and breaking down cultural and financial barriers. We work closely with community leaders to dispel myths, encourage screening, and promote HPV vaccination. We also advocate for better government funding and expanded insurance to ease the financial burden on women.
One of our biggest successes has been helping to push for Nigeria’s HPV vaccination programme. which has reached over 13 million girls in just a year. I was able to reach out to the Gavi team to work with our government here. It took two years of planning, but Nigeria has now vaccinated over 13 million girls in just over a year. This achievement highlights the impact of collaboration between governments, international partners, and community organisations.
The biggest lesson? Community engagement, strong advocacy, and innovative approaches like mobile screening can make a real difference. Cancer care must be accessible, affordable, and stigma-free – and that takes a collective effort.
What challenges remain in ensuring sustainable progress in cancer care?
Access to decision-makers is an important one. For example, a community worker who understands the needs of women often struggles to reach the Commissioner of Health. There’s a lot of good work happening, but it lacks coordination. Community-based organisations need to present their work in a structured way that policymakers can understand.
What is the key message you would like to share on International Women's Day?
There were many examples of successful programmes, from HIV to maternal health, but the issue is the need for government policies to ensure that these initiatives continue. Everybody has a role to play, and we all must keep playing that role. With concerted efforts at both the community and policy levels, the hope is that more women will gain the access they need to essential cancer services, ultimately saving lives across Africa.
Last update
Thursday 27 March 2025