Prioritising people in cancer care

In the lead-up to World Cancer Day on 4 February, Dr Linda Kollmar, Associate Vice President at MSD, a UICC partner, shares how caring for people with cancer goes beyond their disease, and how applying this approach on a global scale is critically important to affect real change.
World Cancer Day gives me a moment to reflect on the progress that has been made to address this global epidemic. While there have been incredible breakthroughs in cancer care in the last decade, millions of people around the world are diagnosed with cancer every year, and there continue to be vast disparities in the care these patients receive and their corresponding outcomes.
As I reflect, I ask myself – what have we done to support the cancer community? What is our role and are we doing enough? We bring the science to the people, but we know that access is also about other factors such as literacy, stigma, awareness, and demographics. Here, too, we are deliberate and we are active. As a collective community, we need to work together to help ensure those who are diagnosed have access to the quality care they need.
Every person diagnosed with cancer is living their own unique story and has individualised needs. Factors that impact health outcomes, such as where people are born, work and live, affect all aspects of cancer care – which is why it’s critical to put people at the centre of their care – from needs to decisions. We must think about patients within the broader context of their community to empower them with an active voice in their own health and treatment journey.
At MSD, our focus is on advancing innovative science to protect and improve the health of people with cancer. We do this by recognising and learning about barriers to care and working to help reduce those barriers and improve access to care.
We start by supporting people from different backgrounds in addressing their health needs, and by focusing our research to reflect the people we serve. Clinical trials can help show if the medicines are safe and work well for people from all different communities. We are committed to continuously evolving our trial recruitment process to achieve representation across diverse populations, including previously underrepresented groups, people of different ages, sexual orientation and gender identities, and people of different socioeconomic, ethnic and demographic backgrounds. By placing people at the forefront, we are developing programmes and policies that enable access to our clinical trials. We believe diversity in clinical trial representation supports research outcomes that are relevant for more communities around the world.
Another barrier to care is simply how difficult information on cancer and health care can be to understand if you do not work in a healthcare field. Many people struggle with what is called ‘health literacy’ – the ability to find, understand and use information and services – and a lack of understanding could lead to an increased risk of poor health outcomes.
As part of our efforts, we work to create easy-to-understand materials across stages of product development, from clinical trials to labelling and packaging to disease and product educational resources. We have also developed a glossary to help people without medical or scientific training understand more than 1,000 medical healthcare terms and definitions.
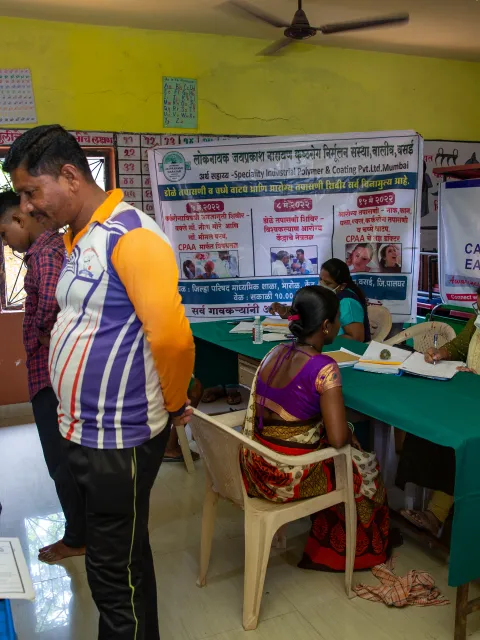
Beyond addressing barriers to care, the implementation of people-centred care means embracing collaboration and connection to ensure everyone is seen as an individual person with needs beyond their disease. Partnerships among healthcare providers, advocacy organisations, healthcare companies, academic institutions and governments are integral to share best practises from different regions meaningfully to advance and provide equitable access to cancer care. We support the broader adoption of people-centred care, including the World Health Organization’s (WHO) initiative to engage people with lived experiences (PWLE) in healthcare decision-making.
WHO has begun piloting PWLE engagement in oncology across six countries in the Mediterranean region. In November of 2024, WHO, in collaboration with Morocco’s Ministry of Health, held a pivotal workshop with multiple patient organisations centred on implementing the WHO PWLE framework to formally include the patient voice in healthcare decision-making. This event identified key priorities such as reducing time to diagnosis and enhancing screening efforts. Attendees committed to reduce stigma, improve access and protect patient rights, and this commitment was supported by the Moroccan government’s pledge to integrate patient representation into policy-making processes. Our company is proud to be a part of this initiative that has sparked essential dialogue across the cancer care continuum, with scientific leaders, healthcare providers, decision-makers and patient advocates aligning on priority areas for individualised patient care and holistic community impact.
Together, our efforts not only strengthen local healthcare systems, but also pave the way for similar advancements around the world. This World Cancer Day and beyond, we need to unite and care for people with cancer beyond their disease to make a difference in their lives and their communities worldwide.
Last update
Wednesday 22 January 2025Share this page