Cervical cancer
Cervical cancer continues to place a heavy burden on women worldwide, especially in regions with limited access to screening and treatment. Cervical cancer is the fourth most common cancer among women globally and currently, one life is lost every two minutes to this disease. Yet it is also one of the most preventable cancers, with HPV vaccination, early detection and timely treatment offering a clear path to reducing cases and deaths.

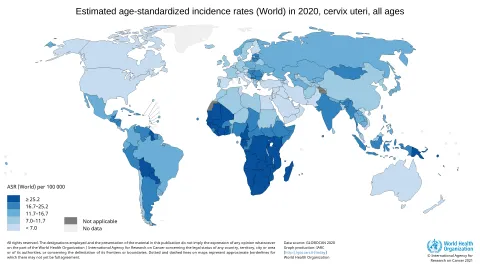
Cervical cancer ranks fourth of all cancers both in terms of incidence and mortality and currently, it is the highest cause of cancer deaths in women in 38 countries.
In 2022, more than 348,000 women died from cervical cancer worldwide and this number is likely to continue to grow, particularly in vulnerable communities. Current data suggests that 94% of all cases occur in low- and middle-income countries, due largely to poor access to screening, early detection and treatment of both pre-cancers and cancer.
However, cervical cancer is one of the most preventable and successfully treatable forms of cancer, if it is detected and diagnosed early, and managed effectively. Like many cancers, the earlier cervical cancer is detected, the higher the chances of survival.
UICC podcast on cervical cancer
In this episode of Let’s talk cancer, Dr Chemtai Mungo from the University of North Carolina, and UICC Young Leader 2021/22 explains the challenges and advances in cervical cancer care and improving access to life-saving services for all populations.
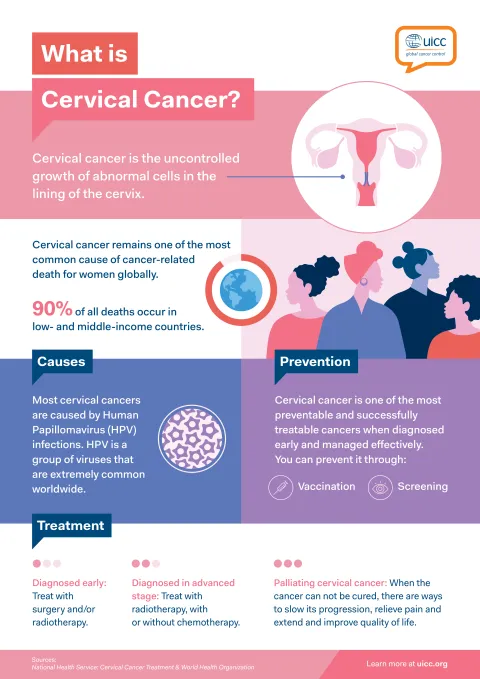
What is cervical cancer?
Cervical cancer is the uncontrolled growth of abnormal cells in the lining of the cervix. The cervix is part of the female reproductive system and is located in the lower part of the womb, forming the opening from the womb to the vagina.
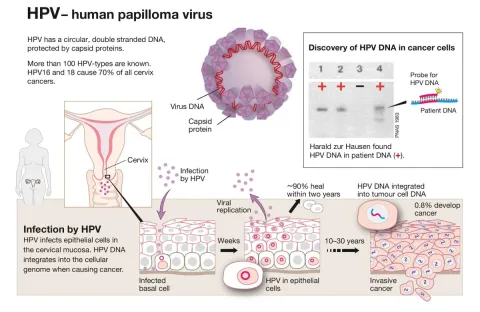
Most cervical cancers are caused by human papillomavirus (HPV) infections. HPV is a group of viruses that are extremely common worldwide. There are more than 100 types of HPV, of which at least 14 are cancer-causing (also known as high-risk types). Two HPV types (16 and 18) cause 70% of cervical cancers and pre-cancerous cervical lesions. There is also evidence linking HPV with cancers of the anus, vulva, vagina, penis and oropharynx. (WHO cervical cancer fact sheet)
There are two main types of cancer of the cervix: squamous cell carcinomas (about 80-90% of cervical cancers) and adenocarcinomas (about 10-20% of cervical cancers).
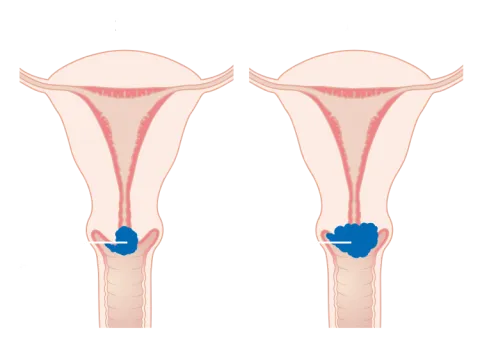
Diagramme showing stage 1B cervical cancer
Author: Cancer Research UK - CC BY-SA 4.0
Addressing and eliminating cervical cancer
Following the call to action in 2018 by the World Health Organization Director General, Dr Tedros Adhanom Ghebreyesus, in 2020, the World Health Assembly passed a resolution, and adopted a strategy aimed at eliminating cervical cancer worldwide as a public health problem.
The Global Strategy identifies the following threshold: cervical cancer would no longer be considered to be a public health problem when all countries reach an annual incidence rate of four cases per 100,000 women or less.
Elimination of cervical cancer could happen within the lifetime of today’s young girls.
A three-pillar approach
The Global Strategy outlines three main pillars to achieving this goal requiring accelerated action in prevention, screening and cancer management, to reach the following targets by 2030:

of girls fully vaccinated with HPV vaccine by 15 years of age

of women are screened with a high-performance test by 35 and 45 years of age, pre-cancerous lesions are treated early

of women identified with cervical disease receive treatment (including treatment of cervical pre-cancer, and invasive cancer)
In order to achieve elimination, action across all three pillars is critical. No single intervention is enough.
It is estimated that by achieving the 90:70:90 targets by 2030, and sustaining these efforts, 74 million new cases of cervical cancer and 62 million deaths in 78 low- and middle-income countries will be averted by 2120.
Mandated by the World Health Assembly resolution in 2025, the 17 November marks World Cervical Cancer Elimination Day - the anniversary of the launch of the World Health Organization's (WHO) Global Strategy to accelerate the elimination of cervical cancer as a public health problem.
The Global Strategy and its related targets represent a unique opportunity to drive long-term, sustainable advocacy and save lives.
UICC’s work on cervical cancer
Following the call to action in 2018, UICC directly supported WHO’s efforts to conceive, draft and present the Global Strategy to accelerate the elimination of cervical cancer as a public health problem, which was launched on 17 November 2020.
Since then, UICC has actively supported the WHO-led Cervical Cancer Elimination initiative, working with its diverse and global membership to assist countries in achieving the 90:70:90 targets for vaccination, screening and treatment, and continuing to maintain a spotlight on cervical cancer elimination, leveraging its global platforms and harness its convening role across sectors to drive global impact.
In fulfilment of these commitments, UICC is delivering and provides a series of activities, opportunities and projects, working with partners, members and organisations around the world to support collective progress towards the 2030 targets.

A space for professionals in the field of cervical cancer elimination to connect, collaborate, share insights and support one another.
Virtual Dialogue - Advocacy in action: the role of civil society in cervical cancer elimination
Virtual Dialogue - Navigating Gavi: Supporting CSOs in advancing access to HPV vaccination
Virtual Dialogue: Implementing 70:90 – Ensuring scale and sustainability






What is cervical cancer?
Cervical cancer is a growth of abnormal cells that begins in the cervix, the lower part of the uterus that connects to the vagina. Most cases of cervical cancer are caused by certain strains of the human papillomavirus (HPV), a common sexually transmitted infection.
What are the signs of cervical cancer?
Early stages of cervical cancer may not cause symptoms. However, advanced stages can lead to abnormal vaginal bleeding between periods, pain during intercourse, pelvic pain, unusual discharge, weight loss, fatigue and loss of appetite, vaginal discomfort and swelling in the legs. It’s crucial to undergo regular screening to detect the disease in its early stages.
Can cervical cancer be prevented?
Cervical cancer can be prevented through vaccination against HPV, regular screening (Pap smear and HPV test), practising safe sex, and avoiding smoking.
High-quality evidence assessing single-dose HPV vaccination suggests that implementing a single-dose schedule is scientifically sound and provides the greatest public health benefit. The primary target of vaccination is girls aged 9-14, prior to the start of sexual activity. The vaccination of secondary targets such as boys and older females is recommended where feasible and affordable.
How can cervical cancer be detected?
Precancers rarely cause symptoms, which is why regular cervical cancer screening is important, even if you have been vaccinated against HPV. Women should be screened for cervical cancer every 5-10 years starting at age 30. Women living with HIV should be screened every 3 years starting at age 25. The WHO Global Strategy for Cervical Cancer Elimination recommends at least two lifetime screens using a high-performance HPV test - first by age 35 and again by age 45.
Screening can be done through Pap smears or HPV tests, both of which are effective methods for detecting precancerous changes. In addition, self-collection of a sample for HPV testing, which may be a preferred option for many women, has been shown to be as reliable as samples collected by healthcare providers.
Who is at risk of developing cervical cancer?
All women are at risk of developing cervical cancer, especially those who have persistent infection with high-risk types of human papillomavirus (HPV). The highest burden occurs in low- and middle-income countries, where access to HPV vaccination, screening, and treatment remains limited. Women living with HIV are also at much greater risk, about six times more likely to develop cervical cancer than the general population. Other contributing factors include early sexual activity, multiple pregnancies, smoking, long-term use of hormonal contraceptives, and weakened immune systems.
What treatment are available for cervical cancer?
Treatment of precancerous lesions is a simple and effective procedure that prevents cervical cancer. Treatment is quick, generally painless, and rarely cause complications. After visual inspection or colposcopy to locate the lesion, treatment may involve thermal ablation or cryotherapy to destroy abnormal cells, or minor surgical procedures such as large loop excision of the transformation zone (LLETZ) or cone biopsy to remove the affected tissue.
Early-stage cervical cancer can often be treated successfully, while more advanced cases may require surgery, radiation therapy, chemotherapy, or a combination of these, along with palliative care to relieve symptoms and improve quality of life.
How is cervical cancer addressed at a global level?
In 2020, the World Health Assembly adopted a resolution and a Global strategy to eliminate cervical cancer as a public health problem. The World Health Organization (WHO) defines elimination as reducing the number of new cases to four or fewer per 100,000 women each year.
To reach this goal, the strategy sets three key targets for 2030: 1) ensuring that 90% of girls are vaccinated against HPV by age 15, 2) 70% of women are screened with a high-quality test by ages 35 and 45, 3) and 90% of women with cervical disease receive appropriate treatment. These efforts aim to put all countries on the path toward eliminating cervical cancer in the coming decades.
Latest news and blog articles on cervical cancer
Cameroon’s people-centred HPV vaccination campaign builds trust through mothers, churches, and community health workers

Podcast "Let's Talk Cancer" – Providing supportive care in Egypt

Nigeria's path to cervical cancer elimination: Challenges, data, and people-centred care


UICC works closely with the World Health Organization (WHO), other UN agencies and partners towards the elimination of cervical cancer as a public health problem.
This page regroups important resources such as infographics, videos, documents and links related to cervical cancer elimination.

The ICCP Portal features additional resources on cervical cancer prevention and control such as National Cervical Cancer Control Strategies and Plans.

In 2020, the WHO set the 90-70-90 targets aiming to eliminate cervical cancer by 2030. Vaccinate 90% of girls, screen 70% of women, treat 90% with cervical disease. Expected benefits include a 42% reduction in cervical cancer rates by 2045 and preventing over 74 million new cases by 2120, with 300,000 deaths averted by 2030.
Global strategy for the elimination of cervical...

UICC analysed the role of civil society organisation (CSOs) in promoting HPV vaccination for cervical cancer elimination, identified barriers, and launched the summary on the Global Strategy's third anniversary.
Landscaping the engagement of cancer organisations...
Last update
Wednesday 11 February 2026