Building survivorship care for children with cancer in Uganda
Dr Derrick Bary Abila of the Uganda Cancer Institute speaks about his recent UICC Technical Fellowship at St. Jude Children’s Research Hospital in the US, applying models of survivorship care for children treated with cancer in Uganda, from structuring follow-up clinics to tailoring research tools to study late health effects.

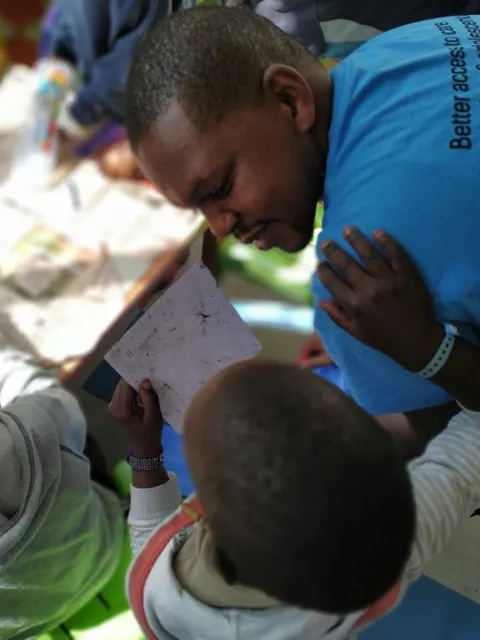
Dr Derrick Abila (Left) completed a four-week Fellowship at St Jude Children’s Research Hospital, Memphis, Tennessee – here with R. Elyse Heidelberg, Assistant Member and Clinical Psychologist at St Jude – focused on how childhood cancer survivorship programmes and addressing the long-term effects of childhood cancer.
HIGHLIGHTS
-
Dr Derrick Bary Abila of the Uganda Child Cancer Foundation at the Uganda Cancer Institute completed a UICC Technical Fellowship at St. Jude Children’s Research Hospital in the United States, where he observed survivorship programmes such as the ACT Clinic, SJLIFE, and CCSS.
-
He explored approaches to structuring follow-up clinics, tailoring research tools to study late health effects, and strengthening grant-writing for survivorship research.
-
He shared Uganda’s experience of the social and financial barriers that limit access to treatment, contributing to a two-way exchange with colleagues at St. Jude.
-
He is now applying these insights in Uganda through paediatric oncology training, school-based awareness programmes, and survivor-led initiatives such as ‘Heroes Beyond Cancer’.
When Dr Derrick Bary Abila first entered a paediatric oncology ward of the Uganda Cancer Institute (UCI) during a medical school elective, he saw the particular challenges facing children with cancer, an experience that shaped his focus on paediatric oncology. “In adults, you can sometimes link cancer to risk factors such as tobacco use during their lifetime, but in children, it can’t be tied to any lifetime risk factors,” he said in a conversation with UICC. “That really triggered my interest in paediatric oncology.”
Now a medical doctor at the Uganda Cancer Institute (UCI), a UICC member, and Research Program Manager at the Uganda Child Cancer Foundation, Abila recently completed a UICC Technical Fellowship at St. Jude Children’s Research Hospital in the US, also a UICC member.
The four-week fellowship visit focused on how childhood cancer survivorship programmes are designed and run, encompassing the After Completion of Therapy (ACT) Clinic, which provides structured follow-up for children five years after diagnosis, and research into the long-term effects of childhood cancer through the St. Jude Lifetime (SJLIFE) cohort study and the Childhood Cancer Survivor Study (CCSS), which track thousands of survivors over decades.
His aim is to improve the quality of life for children who have had cancer in Uganda, by building collaborative networks, improving survivorship clinic structures at UCI, developing context-appropriate tools to track late health effects, and strengthening grant writing and management for future survivorship research.
While survival rates for childhood cancer are estimated at around 80% in high-income countries, in low- and middle-income countries, survival can be less than 30%.
There are indeed significant barriers to accessing effective care, beginning with recognising the early signs of childhood cancer. “Specialists focused on childhood cancer are few, and symptoms often overlap with common illnesses, which can mislead parents and frontline health workers,” said Abila.
Even once a diagnosis is made, families face obstacles in continuing treatment. Public hospitals provide free cancer treatment and medicines, but other costs quickly accumulate. “When someone has to travel more than 100 kilometres from home, they may struggle with transport, accommodation near treatment centres, and costs of non-cancer medicines – expenses that are not covered by public institutions such as UCI,” he explained.
These pressures make it difficult to remain on therapy. “A good number can start treatment, but many will not complete it. They either abandon or miss appointments because of those extra costs, which are mostly social rather than medical,” Abila said. The Uganda Child Cancer Foundation (UCCF), through its patient support program, holds an Annual Childhood Cancer Color Run to raise funds to support in covering out-of-pocket costs, with the 2025 edition focusing on raising funds to build a patient hostel (lodging).
The Uganda Cancer Institute began procuring drugs directly from pharmaceutical companies, which improved their availability. The Ministry of Health has since added these medicines to the national essential medicines list, and they are now provided free of charge at UCI.
UCI is also seeking to address issues of earlier diagnosis and continuity of care. The organisation has notably launched a two-year paediatric oncology fellowship to expand the number of specialists able to diagnose and treat childhood cancers, helping to reduce delays and improve outcomes. The programme is training paediatricians in oncology so that more children can access care closer to home, rather than relying on the small number of oncologists at UCI.
Community awareness programmes also play an important role. The Uganda Child Cancer Foundation runs the ‘Children Caring About Cancer’ (3C) initiative in more than 250 schools across Uganda having 3C clubs, educating students about the signs and symptoms of cancer and equipping them to share this knowledge with their communities.
From successful treatment to managing life after
“While we still face many challenges in Uganda to see more children diagnosed and treated successfully, we don’t have to wait for survival rates to reach 80% before we start thinking about survivorship,” said Abila.
UCI runs a weekly long-term follow-up clinic for children who have completed therapy, but this service is still developing. “Patients do come, but there is no clear structure,” Abila explained. “We needed to understand who should be enrolled, how referrals should work, and what standard assessments to carry out at each visit.”
Abila applied for a UICC Technical Fellowship to observe survivorship practice at St. Jude Children’s Research Hospital in Memphis. “St. Jude has a very robust childhood cancer survivorship programme,” he said, referring to the ACT clinic, established in 1984. Eligibility there typically includes being at least five years from diagnosis. Annual follow-up continues until the age of 18, or 10 years after treatment, whichever comes later.
During a month-long placement, Abila rotated with paediatric oncologists and fellows, observed clinic flow, assessments and referrals, and studied how appointments and reminders are scheduled. “Sometimes the devil’s in the details… If you don’t have the right tools, the patients just go through,” he said. Reviewing records from UCI’s clinic, “the summary notes of the visit [were] like one page,” underscoring the need for standard tools.
The Technical Fellowship visit also focused on research infrastructure. At St. Jude, Abila saw how survivorship care is informed by decades of research, including the SJLIFE and CCSS studies. “Evidence is key,” he said, “but most survivorship guidelines are not tailored to our setting. If we apply these guidelines directly, they may not reflect the realities of children in Uganda. The medications and dosages we use are not always the same, so the late health effects we see may also differ. That is why we must generate our own data and evidence.”
Working with mentors at St. Jude, such as Melissa M. Hudson, Matthew J. Ehrhardt, Daniel A. Mulrooney, Nickhill Bhakta, and many others, helped adapt research tools and co-developed a grant proposal to establish a local cohort at UCI. “The research aspect of our clinic will help us generate evidence on late health effects specific to Uganda,” Abila explained. “That way, follow-up care will be based on evidence from our context and truly meet the needs of our patients.”
Beyond clinical follow-up, survivorship in Uganda also means addressing the return to daily life. “The end of oncology follow-up at around two to three years post-treatment can be destabilising,” Abila explained. “Children and young adults naturally get attached to the nurses and doctors who treated them – but who now have to care for other patients. Some will call and ask, ‘Have you forgotten about me?’”
The Uganda Child Cancer Foundation (UCCF) initiated its Heroes Beyond Cancer project, organising workshops for survivors, parents, and health workers where they can discuss the long-term medical, social and psychological effects of childhood cancer. It also equips people who have had cancer with storytelling and public speaking skills to raise awareness, fight stigma, and promote psychosocial support for people who are living with or have experienced cancer.
People who have had cancer as children are themselves are at the forefront of these efforts – the director of UCCF is a survivor of childhood cancer – underscoring the importance of peer support and visibility.
Costs and coverage remain a major concern. Just as transport and accommodation can make it difficult to stay on treatment, similar costs arise after therapy ends. “Post-treatment needs such as audiology or other specialist care are available in the referral system and covered by public healthcare facilities, but travel and housing costs are not,” Abila explained.
Abila noted that knowledge was shared in both directions between him and the team at St. Jude's. “While St. Jude’s programmes are well resourced, they also serve low-resource communities in the USA and globally,” Abila observed. “How we respond to the needs for transport, accommodation, and psychosocial support in Uganda can inform decisions in Memphis and communities that St Jude serves.”
These challenges highlight why survivors themselves must be involved in shaping solutions. Peer support not only reduces isolation but also strengthens advocacy for practical changes.
UCI and UCCF are members of St. Jude Global, and Abila’s fellowship created further opportunities for mentorship and collaboration. “The team at St. Jude pledged to continue supporting mentorship during the project I submitted for an early career award from the Thrasher Research Fund, and in other future work focused on survivorship,” he said.
Immediate next steps are already underway. “We had a meeting last week to streamline what’s next in survivorship care in Uganda,” Abila said. He also pointed to the survivorship workshop held on the sidelines of the 5th Uganda Conference on Cancer & Palliative Care in Kampala, Uganda, that brought together paediatric oncologists, gynaecologists focused on onco-fertility, such as Dr Anthony Kayiira, parents, and people who had cancer during childhood. “I was able to share the outcomes of the fellowship there as well and developed next steps for survivorship care in Uganda.”
Last update
Thursday 02 October 2025