Preventing cancer through vaccination: progress, promise, and key trials
Cancer vaccines, once a distant goal, are edging closer to reality with promising trials such as LungVax, which aims to protect high-risk individuals using cutting-edge mRNA technologies, and treatment vaccines for skin and head and neck cancers.

HIGHLIGHTS
- Cancer vaccines are being developed both to prevent cancer and to treat it, building on research dating back several decades and the success of mRNA vaccines during the COVID-19 pandemic.
- LungVax, backed by Cancer Research UK, a UICC member, and CRIS Foundation, targets early-stage lung cancer signals and will be trialled in 2026 on 3,000 high-risk participants aged 55-74 (current or former smokers with a significant history of tobacco use).
- Therapeutic vaccines for melanoma and HPV-related head and neck cancers are in advanced trials, potentially becoming NHS treatments in the UK within five years.
- Challenges remain – production costs, logistics, and long-term efficacy tracking – especially for personalised approaches.
There has been a recent spate of promising news around cancer vaccines, highlighting clinical trials under way or planned for vaccines targeting melanoma, head and neck, and lung cancers. The potential of these vaccines lies in their ability to engage the immune system in new and targeted ways, offering hope for improved outcomes for cancers that are difficult to treat or detect early.
Researchers are exploring both therapeutic uses to treat existing cancers, and prophylactic approaches designed to prevent cancer from developing in the first place.
The idea of using the immune system to prevent or treat cancer dates back over a century. Early examples include Coley’s toxins in the 1890s, based on observations of tumour regression after bacterial infections. This work arguably laid the groundwork for modern cancer immunotherapy.
The early 2000s saw a breakthrough in a separate area, with the development of prophylactic or preventative vaccines, not against the cancer itself but against viruses linked to cancer, notably the human papillomavirus (HPV) vaccine to prevent cervical cancer, and hepatitis B to prevent liver cancer. These have proven highly effective and are now part of standard immunisation programmes in many countries.
Around the same time, researchers began focusing on therapeutic vaccines that could treat existing cancer by stimulating the immune system to attack tumour cells directly. Among the most studied were dendritic cell vaccines, which harvest a type of immune cell that helps coordinate immune responses, exposing them to cancer antigens in the laboratory, then returning them to the body where they can help trigger a targeted immune attack on the tumour.
Production proved to be complex, time-consuming, and costly, however, and clinical response rates have generally been modest. The vaccines showed particular promise for melanoma in early trials, but ultimately have not yielded convincing outcomes.
What is now gaining media attention and showing real promise for cancer prevention and treatment are mRNA-based vaccines. The underlying technology has been known for more than 60 years, and cancer vaccine research using mRNA has been under way for at least two decades, but they were proving to be difficult to stabilise and required further development of safe and effective delivery systems before broader use became feasible. Then came the COVID-19 pandemic.
“The pandemic created an urgent need and provided the funding, scale, and public focus for researchers to prove that mRNA vaccines could work in real time, on a global scale,” said Sophie Wedekind, Digital News Editor at Cancer Research UK (CRUK), in a conversation with UICC. “It significantly removed many of the scientific, financial, and regulatory barriers that had previously slowed down the development, production, and safe delivery of this technology.”
Targeting early signals in lung cancer through vaccination
The mRNA enables researchers to “use it as a tool for our own immune to target cancer cells through vaccines,” according to Wedekind, allowing for a highly targeted immune response.
This technology is being harnessed in the research and development of a preventive lung cancer vaccine, LungVax. It is supported by GBP 1.7 million in funding from CRUK, a UICC member organisation, and the CRIS Cancer Foundation.
Developed by the University of Oxford, University College London, and the Francis Crick Institute, the vaccine uses a viral vector platform to deliver neoantigens – proteins produced by early-stage cancer cells – that help the immune system detect and respond to cancer development.
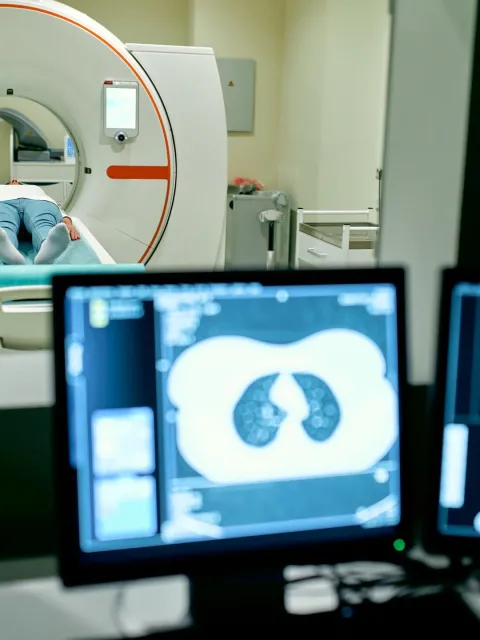
LungVax is being explored as a complement to screening, offering an additional safeguard for those at greatest risk of developing lung cancer. The vaccine will be trialled among 3,000 individuals aged 55–74 who are already enrolled in the NHS Lung Health Check programme. They are defined as high risk due to their history of smoking, including current or former smokers with a significant tobacco exposure, such as a 30 pack-year history.
By working with individuals already undergoing low-dose CT scans, researchers aim to combine early detection with vaccine-based prevention. The vaccine introduces cancer-specific signals at an early stage, helping the immune system recognise and respond to developing tumours before they progress.
“Cancer is a disease of our own bodies, so it can be difficult for the immune system to recognise cancer cells as a threat,” said Sophie Wedekind. “The idea behind this preventative vaccine is to introduce cancer-specific signals early, so the immune system knows what to look for if a tumour starts to form.”
She added that enthusiasm from both researchers and trial participants is contributing to faster progress. “The researchers have said it’s been a very positive trial to be a part of, and there is a level of enthusiasm that comes with it.”
And how soon will researchers know if the vaccine works? “Certainly, the key challenge is that we need to wait a long time to see if cancer develops or not and assess the vaccine’s efficiency,” said Sophie Wedekind. “In the meantime, researchers monitor immune responses or biological markers in high-risk groups to assess whether the vaccine is having the intended biological effect.”
Wedekind emphasises that while a vaccine could provide meaningful protection for people already affected by long-term exposure, stopping smoking remains the most effective way to reduce lung cancer risk and related mortality.
Therapeutic cancer vaccines: targeting disease already present
The other major area of cancer vaccine research focuses on therapeutic vaccines – designed to treat cancer after diagnosis. Rather than preventing disease, these vaccines aim to prompt the immune system to recognise and destroy cancer cells, potentially slowing tumour growth, preventing recurrence, or improving the effectiveness of other treatments such as immunotherapy or chemotherapy.
Beyond LungVax, CRUK is supporting a range of other trials in the UK. Among them is a personalised mRNA-based vaccine for advanced melanoma, now in the final phase of trials and expected to become the first therapeutic cancer vaccine available through NHS clinics. Another candidate – a head and neck cancer vaccine targeting HPV-related tumours – was recently fast-tracked into clinical trials as part of the NHS Cancer Vaccine Launch Pad.
Researchers are hopeful that the first generation of cancer vaccines – including therapeutic options for skin cancer and preventative approaches for lung cancer – could become available within the next five years.
Significant challenges remain. Personalised vaccines demand sophisticated manufacturing processes and logistics, including cold chain storage and tight integration with clinical services. Costs are high, and regulatory pathways for emerging technologies must evolve to assess safety, efficacy, and equity in access.
CRUK is also supporting research into more generalised vaccine technologies, which may address some of these challenges. One such effort, led by the company Infinitopes, aims to identify shared molecular targets across tumour types – a potential step towards reducing the cost and complexity of vaccine production by lowering reliance on fully personalised approaches.
Last update
Friday 22 August 2025