Bridging the divide: financing cancer care to achieve true universal health coverage
Marking Universal Health Coverage (UHC) Day on 12 December, Sarbani of the UICC-led Access to Oncology Medicines (ATOM) Coalition writes about how innovative health financing strategies could transform access and equity under UHC in LMICs that face critical gaps in cancer care financing.
The WHO estimates that only 39 per cent of universal health care (UHC) benefit packages worldwide include cancer care, and this falls to 28 per cent when palliative care is included. LMICs bear the most significant gaps in cancer care coverage, constrained by limited public funding and competing health demands.
Financial protection lies at the heart of UHC, whereby all people can benefit from quality health services, and represents one of its ultimate goals, with health financing policies shaping how well people are protected.
Lack of coverage has multiple deadly impacts for households and communities in LMICs. Over 70% of cancer deaths reported by the World Health Organization (WHO) occurring in regions where UHC does not offer financial protection for cancer care. For instance, Africa's cancer mortality-to-incidence ratio (0.67) is double than that in wealthier nations (0.33).
Key factors include funding gaps, which can delay diagnosis and treatment, including access to affordable routine screening to detect cancers earlier. Then treatment costs often push people into poverty or deeper poverty, referred to as financial toxicity.
This is why UICC’s new World Cancer Declaration 2025-2035 includes explicit targets on health financing, notably that by 2035, 50% of countries must include essential cancer services in universal health coverage (UHC) packages.
How can LMICs increase funding for cancer care and move closer toward UHC?
The financing of health systems in LMICs is characterised by a mix of sources, including:
- Government expenditure (through general taxation or earmarked funds);
- Out-of-pocket (OOP) payments by individuals at the point of care, where medical services (including diagnosis, treatment, monitoring, and supportive care) are directly given at the time and place of patient interaction;
- External donour funding and development assistance; and
- Health insurance schemes, both public and private.
Changing the pyramid of cancer financing in LMICs
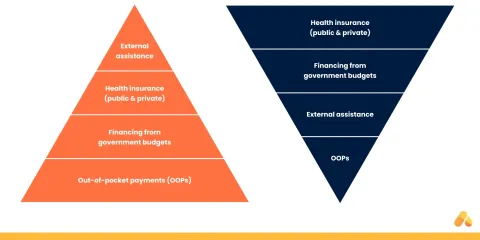
Figure showing the current structure of cancer financing in LMICs (left) and a suggested more sustainable model (right). By author.
Unfortunately for many individuals as the figure above shows, paying out of pocket (OOP) remains their only way to access cancer care services. The NCD Alliance and George Institute report, Paying the Price, found that: “Cancer care is one of the NCDs most likely to cause catastrophic out-of-pocket (OOP) spending — treatment costs are often the single most significant expense and can exceed the catastrophic threshold.
The ability of governments to mobilise and pool revenues and taxes is crucial for financing essential cancer care. In contrast to wealthier nations with robust insurance systems, LMICs continue to lag, with universal health insurance coverage reaching only a small share of their populations.
Many governments are actively seeking ways to expand public health insurance; however, these efforts are facing challenges due to the size of the informal economy, where people work without formal contracts or payroll systems, making it challenging to collect contributions for public insurance systems.
As for private insurance markets, they remain underdeveloped, even with the growth of a middle class, constrained by affordability issues, limited product offerings, and a lack of trust or regulation that would make private coverage a viable option for most people.
Finally, external assistance for financing cancer care – in the form of financial support from international donors, development agencies, global health initiatives, or philanthropic organisations – has always been small in LMICs and nowhere near the scale of financing for HIV/AIDS, malaria, TB, vaccines, and maternal and reproductive health.
To sustainably fund cancer care and meet the needs of people living with cancer and their families, I believe a new funding and financing pyramid is necessary.
Transitioning to a new pyramid
In this pyramid, public and private health insurance play a significant role in financing cancer treatment through pre-paid, pooled funds. Instead of funding hospitals directly, governments can assist low-income households by contributing to public health insurance. The fund selects evidence-based treatments and covers essential elements of cancer care. Health insurance funds contract with health facilities to ensure quality cancer care and hold providers accountable for better outcomes.
Private health insurance plays a key supplementary role in funding additional treatments (over and above the public insurer's basic package). Government financing for cancer control prioritises accurate costing of national plans, mobilising resources, generating evidence for cost-effective interventions, subsidising health insurance for low-income households, and strategically allocating funds across all areas of cancer care.
External support plays a catalytic role in improving cancer care, including fostering public-private partnerships to increase access to cancer medicines and diagnostics, sharing best practices, including in health financing, and strengthening health systems. Public-private partnerships such as UICC’s Access to Oncology Medicines (ATOM) Coalition, and St. Jude's programme for childhood cancer medicines, serve as examples. However, their success depends on countries adequately funding cancer care to strengthen and optimise the health system's ability to deliver services through effective financing mechanisms.
Finally, OOP payments will be marginal, focused more on deterring unnecessary treatments.
Case studies
The ATOM Coalition recently completed four case studies that highlight how countries in different WHO Regions (Africa, Europe and Asia) are advancing health financing for cancer care. These case studies highlight the evolution of many of the concepts discussed above and serve as a best practice regarding policy recommendations for the future.
The following actions are recommended to promote sustainable financing and equitable access to cancer care, including medicines and diagnostics in LMICs:
-
Increase domestic funding for cancer services in national budgets, aligned with priorities outlined in the country's cancer control plan. Ensure that these funds are planned over several years, to ensure continuous, stable financing over several years, and the implementation of the national cancer strategy
-
Use domestic funds to expand coverage, including health insurance coverage for comprehensive oncology services and making sure they are affordable and accessible for traditionally underserved and vulnerable populations
-
Encourage joint efforts among countries to pool procurement (i.e. combine purchasing power to negotiate better prices and supply terms) and align regulatory processes
-
Encourage public-private partnerships to strengthen cancer care delivery by leveraging shared resources, expertise, and infrastructure
-
Support cancer registries and data collection for evidence-based decisions
-
Involve civil society organisations and patient advocacy in policy development and monitoring.
Last update
Thursday 11 December 2025Share this page


